Dry eye is a really common condition caused by a problem with your tears.
When you blink you leave a thin layer, called the tear film, over the front of your eye. The balance of tear production and tear loss [through drainage and evaporation] maintains the moisture level in the eyes. When this balance is not sustained, dry spots appear on the surface of the eye and cause irritation.
What are the symptoms of dry eye?
- Stinging or burning eyes
- Scratchiness/ gritty feeling
- Stringy mucus in or around the eyes
- Eye irritation from smoke or wind
- Excess tearing: reflex tearing due to dryness Redness
What causes dry eye syndrome?
Age related
Systemic autoimmune diseases: which reduce the tear production
Excessive evaporation of tears: caused by meibomitis, which results from infection and inflammation of the meibomian glands in the eyelids. People with unusually large eyes, as well as those who suffer from thyroid disease, may also experience dry eye syndrome caused by excessive evaporation, draft of the air conditioner
Drug related: antibiotics, antihistamines, diuretics, and anti-diarrheals
Hormonal changes
Computer vision syndrome
Eye allergy
How is dry eye diagnosed?
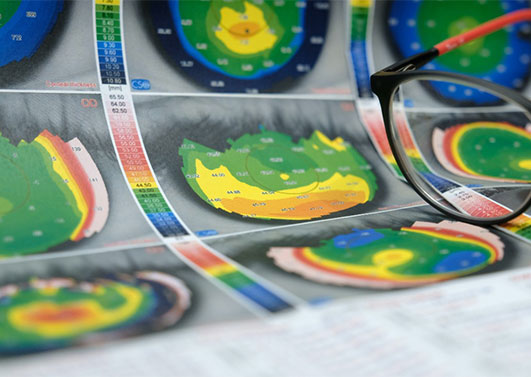
Detailed work up for dry eye assessment, including tear film analysis, surface staining, meibography, etc
How are dry eyes treated?
Type and duration of the treatment depends on the cause of your dryness.
Often simple lubricating drops, removing the aggravating risk factor, warm compresses and eye ointments may be enough.
However, customized treatment plans with lifestyle modifications, consultation for systemic disorders, and surgical interventions including punctal plugs, mucous membrane grafts, conjunctivoplasty, and minor salivary gland transplantation procedures may be necessary for severe dry eye disease.
Click here to view the profile of our corneal surgeon.
What is Keratoconus?
Keratoconus is a progressive ectasia or thinning of the cornea, which is accompanied by an increase in the curvature of the cornea, making it irregular and steep.
Keratoconus occurs in approximately one in 2,000 individuals, typically beginning in puberty and progressing into the mid-30s.
Why does it happen?
The internal bonds linking the different layers of the cornea are weakened, due to genetic or inflammatory conditions. It is often associated with allergy of the eye and increased eye rubbing.
How is it treated?
Keratoconus assessment and customized management using various contact lenses (Rose K, Mini Scleral, Hybrid or Scleral lenses). Intra Corneal Ring Segments (INTACS) using femtosecond laser, Corneal Collagen Crosslinking, Stromal augmentation procedure, Topography guided PRK with accelerated cross linking, and Deep Anterior Lamellar Keratoplasty (DALK) or Penetrating Keratoplasty procedures.
What is it?
A cornea transplant replaces diseased or scarred corneal tissue with healthy tissue from an organ donor.
Types of corneal transplants?
Currently, cornea transplant has undergone many advances and involves layer by layer transplants, which have highly increased the success chances of this operation.
Based on the layer of the cornea that is damaged and replaced, it can be full-thickness or Partial-thickness (LAMELLAR) surgery.
In full thickness or Penetrating Keratoplasty, the entire diseased cornea is removed and replaced with donor tissue of full thickness of the corneal button.
LAMELLAR surgeries are advanced surgeries, where only the damaged tissue is replaced. i.e. either only the front of the cornea or the back of the cornea. This basically means that one donor cornea can be used for 2 different surgeries and help 2 individuals gain sight !
DALK- Deep Anterior Lamellar Keratoplasty and DSEK- Descemet’s Stripping Endothelial Keratoplasty are advanced types of corneal transplants.
When Do You Need A Cornea Transplant?
If your cornea is damaged due to eye disease or eye injury, it can become swollen, scarred or severely misshapen and distort your vision.